 W
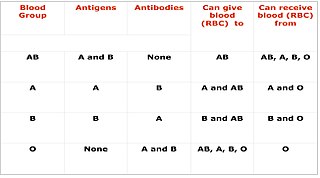
WThe ABO blood group system is used to denote the presence of one, both, or neither of the A and B antigens on erythrocytes. In human blood transfusions it is the most important of the 38 different blood type classification systems currently recognized. A mismatch in this, or any other serotype, can cause a potentially fatal adverse reaction after a transfusion, or an unwanted immune response to an organ transplant. The associated anti-A and anti-B antibodies are usually IgM antibodies, produced in the first years of life by sensitization to environmental substances such as food, bacteria, and viruses.
 W
WAnemia is a decrease in the total amount of red blood cells (RBCs) or hemoglobin in the blood, or a lowered ability of the blood to carry oxygen. When anemia comes on slowly, the symptoms are often vague and may include feeling tired, weakness, shortness of breath, and a poor ability to exercise. When the anemia comes on quickly, symptoms may include confusion, feeling like one is going to pass out, loss of consciousness, and increased thirst. Anemia must be significant before a person becomes noticeably pale. Additional symptoms may occur depending on the underlying cause.
 W
WApheresis is a medical technology in which the blood of a person is passed through an apparatus that separates out one particular constituent and returns the remainder to the circulation. It is thus an extracorporeal therapy.
 W
WAquaporin 3 is the protein product of the human AQP3 gene. It is found in the basolateral cell membrane of principal collecting duct cells and provides a pathway for water to exit these cells. Aquaporin 3 is also permeable to glycerol, ammonia, urea, and hydrogen peroxide. It is expressed in various tissues including the skin, respiratory tract, and kidneys as well as various types of cancers. In the kidney, aquaproin 3 is unresponsive to vasopressin, unlike Aquaporin 2. This protein is also a determinant for the GIL blood group system.
 W
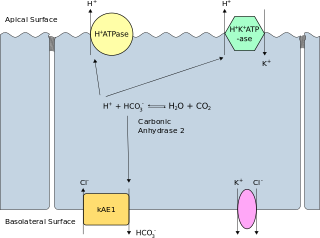
WBand 3 anion transport protein, also known as anion exchanger 1 (AE1) or band 3 or solute carrier family 4 member 1 (SLC4A1), is a protein that is encoded by the SLC4A1 gene in humans.
 W
WBasigin (BSG) also known as extracellular matrix metalloproteinase inducer (EMMPRIN) or cluster of differentiation 147 (CD147) is a protein that in humans is encoded by the BSG gene. This protein is a determinant for the Ok blood group system. There are three known antigens in the Ok system; the most common being Oka, OK2 and OK3. Basigin has been shown to be an essential receptor on red blood cells for the human malaria parasite, Plasmodium falciparum.
 W
WBleeding, also known as a hemorrhage, haemorrhage, or simply blood loss, is blood escaping from the circulatory system from damaged blood vessels. Bleeding can occur internally, or externally either through a natural opening such as the mouth, nose, ear, urethra, vagina or anus, or through a wound in the skin. Hypovolemia is a massive decrease in blood volume, and death by excessive loss of blood is referred to as exsanguination. Typically, a healthy person can endure a loss of 10–15% of the total blood volume without serious medical difficulties. The stopping or controlling of bleeding is called hemostasis and is an important part of both first aid and surgery. The use of cyanoacrylate glue to prevent bleeding and seal battle wounds was designed and first used in the Vietnam War. Today many medical treatments use a medical version of "super glue" instead of using traditional stitches used for small wounds that need to be closed at the skin level.
 W
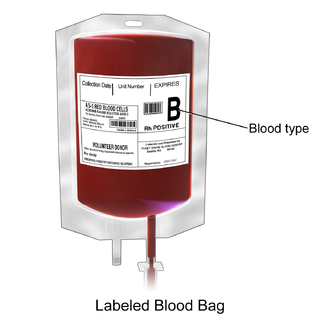
WA blood donation occurs when a person voluntarily has blood drawn and used for transfusions and/or made into biopharmaceutical medications by a process called fractionation. Donation may be of whole blood, or of specific components directly. Blood banks often participate in the collection process as well as the procedures that follow it.
 W
WBlood plasma is a yellowish liquid component of blood that holds the blood cells of whole blood in suspension. It is the liquid part of the blood that carries cells and proteins throughout the body. It makes up about 55% of the body's total blood volume. It is the intravascular fluid part of extracellular fluid (all body fluid outside cells). It is mostly water (up to 95% by volume), and contains important dissolved proteins (6–8%) (e.g., serum albumins, globulins, and fibrinogen), glucose, clotting factors, electrolytes (Na+, Ca2+, Mg2+, HCO3−, Cl−, etc.), hormones, carbon dioxide (plasma being the main medium for excretory product transportation), and oxygen. It plays a vital role in an intravascular osmotic effect that keeps electrolyte concentration balanced and protects the body from infection and other blood disorders.
 W
WBlood transfusion is the process of transferring blood or blood products into one's circulation intravenously. Transfusions are used for various medical conditions to replace lost components of the blood. Early transfusions used whole blood, but modern medical practice commonly uses only components of the blood, such as red blood cells, white blood cells, plasma, clotting factors, and platelets.
 W
WA blood type is a classification of blood, based on the presence and absence of antibodies and inherited antigenic substances on the surface of red blood cells (RBCs). These antigens may be proteins, carbohydrates, glycoproteins, or glycolipids, depending on the blood group system. Some of these antigens are also present on the surface of other types of cells of various tissues. Several of these red blood cell surface antigens can stem from one allele and collectively form a blood group system.
 W
WBlood typing is a medical laboratory test used to identify the antigens on a person's red blood cells, which determine their blood type. Routine blood typing involves determining the ABO and RhD type, and is performed before blood transfusions to ensure that the donor blood is compatible. It is also used to help diagnose hemolytic disease of the newborn, a condition caused by incompatibility between the blood types of a mother and her baby. ABO typing involves both identification of ABO antigens on red blood cells and identification of ABO antibodies in the plasma. Other blood group antigens, such as the RhC/c and E/e antigens or the K antigen, may be tested for in special situations.
 W
WComplement C4-A is a protein that in humans is encoded by the C4A gene.
 W
WThe CD44 antigen is a cell-surface glycoprotein involved in cell–cell interactions, cell adhesion and migration. In humans, the CD44 antigen is encoded by the CD44 gene on Chromosome 11. CD44 has been referred to as HCAM, Pgp-1, Hermes antigen, lymphocyte homing receptor, ECM-III, and HUTCH-1.
 W
WCD59 glycoprotein, also known as MAC-inhibitory protein (MAC-IP), membrane inhibitor of reactive lysis (MIRL), or protectin, is a protein that in humans is encoded by the CD59 gene. It belongs to the LY6/uPAR/alpha-neurotoxin protein family.
 W
WThe LU domain is an evolutionally conserved protein domain of the three-finger protein superfamily. This domain is found in the extracellular domains of cell-surface receptors and in either GPI-anchored or secreted globular proteins, for example the Ly-6 family, CD59, and Sgp-2.
 W
WCD151 molecule, also known as CD151, is a human gene.
 W
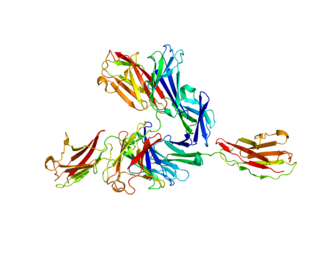
WComplement receptor type 1 (CR1) also known as C3b/C4b receptor or CD35 is a protein that in humans is encoded by the CR1 gene.
 W
WIn transfusion medicine, cross-matching or crossmatching is testing before a blood transfusion to determine if the donor's blood is compatible with the blood of an intended recipient. Cross-matching is also used to determine compatibility between a donor and recipient in organ transplantation. Compatibility is determined through matching of different blood group systems, the most important of which are the ABO and Rh system, and/or by directly testing for the presence of antibodies against the antigens in a sample of donor blood or other tissue.
 W
WComplement decay-accelerating factor, also known as CD55 or DAF, is a protein that, in humans, is encoded by the CD55 gene.
 W
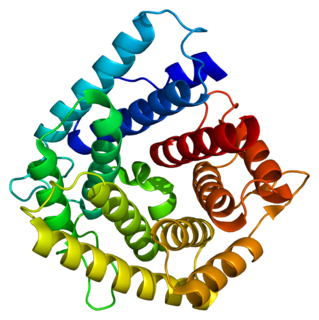
WDuffy antigen/chemokine receptor (DARC), also known as Fy glycoprotein (FY) or CD234, is a protein that in humans is encoded by the ACKR1 gene.
 W
WEmergency bleeding control describes actions that control bleeding from a patient who has suffered a traumatic injury or who has a medical condition that has caused bleeding. Many bleeding control techniques are taught as part of first aid throughout the world, though some more advanced techniques such as tourniquets, are often taught as being reserved for use by health professionals, or as an absolute last resort, to mitigate associated risks, such as potential loss of limbs. To manage bleeding effectively, it is important to be able to readily identify types of wounds and types of bleeding.
 W
WFresh frozen plasma (FFP) is a blood product made from the liquid portion of whole blood. It is used to treat conditions in which there are low blood clotting factors or low levels of other blood proteins. It may also be used as the replacement fluid in plasma exchange. Using ABO compatible plasma, while not required, may be recommended. Use as a volume expander is not recommended. It is given by slow injection into a vein.
 W
WGastrointestinal bleeding, also known as gastrointestinal hemorrhage (GIB), is all forms of bleeding in the gastrointestinal tract, from the mouth to the rectum. When there is significant blood loss over a short time, symptoms may include vomiting red blood, vomiting black blood, bloody stool, or black stool. Small amounts of bleeding over a long time may cause iron-deficiency anemia resulting in feeling tired or heart-related chest pain. Other symptoms may include abdominal pain, shortness of breath, pale skin, or passing out. Sometimes in those with small amounts of bleeding no symptoms may be present.
 W
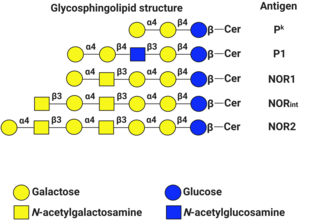
WA globoside is a type of glycosphingolipid with more than one sugar as the side chain of ceramide. The sugars are usually a combination of N-acetylgalactosamine, D-glucose or D-galactose. A glycosphingolipid that has only one sugar as the side chain is called a cerebroside.
 W
WHemolytic disease of the newborn, also known as hemolytic disease of the fetus and newborn, HDN, HDFN, or erythroblastosis foetalis, is an alloimmune condition that develops in a fetus at or around birth, when the IgG molecules produced by the mother pass through the placenta. Among these antibodies are some which attack antigens on the red blood cells in the fetal circulation, breaking down and destroying the cells (hemolysis). The fetus can develop reticulocytosis and anemia. This fetal disease ranges from mild to very severe, and fetal death from heart failure can occur. When the disease is moderate or severe, many erythroblasts are present in the fetal blood, and so these forms of the disease can be called erythroblastosis fetalis.
 W
WThe human leukocyte antigen (HLA) system or complex is a group of related proteins that are encoded by the major histocompatibility complex (MHC) gene complex in humans. These cell-surface proteins are responsible for the regulation of the immune system. The HLA gene complex resides on a 3 Mbp stretch within chromosome 6p21. HLA genes are highly polymorphic, which means that they have many different alleles, allowing them to fine-tune the adaptive immune system. The proteins encoded by certain genes are also known as antigens, as a result of their historic discovery as factors in organ transplants. Different classes have different functions:
 W
WIatrogenic anemia, also known as nosocomial anemia or hospital-acquired anemia, is a condition in which a person develops anemia due to medical interventions, most frequently repeated blood draws. Other factors that contribute to iatrogenic anemia include bleeding from medical procedures and dilution of the blood by intravenous fluids. People may receive blood transfusions to treat iatrogenic anemia, which carries risks for complications like transfusion reactions and circulatory overload.
 W
WDr. Jai Gopal Jolly, famously known as Dr. J. G. Jolly is an Indian physician and Emeritus Professor of the Department of Transfusion Medicine at the Post Graduate Institute of Medical Education and Research, Chandigarh, India. He is an internationally known expert in the field of blood transfusion, who pioneered the voluntary blood donation movement in India, and is regarded as the "Father of Transfusion Medicine in India". He spearheaded the campaign to prohibit sale and purchase of blood from professional donors in India, which was later incorporated into the National Blood Policy of India by the Government of India. He has generated awareness among the masses about the significance of blood donation programmes by observing "Blood Donation Day" on 1 October. This has helped in obtaining adequate quantity of quality blood from voluntary donors. His dedicated work has contributed magnificently to the development and excellence in professional service, research and teaching in the field of Transfusion Medicine in India.
 W
WSamuel Armstrong Lane FRCS was an English surgeon, consulting surgeon to St Mary's Hospital.
 W
WThe Lutheran antigen systems is a classification of human blood based on the presence of substances called Lutheran antigens on the surfaces of red blood cells. There are 19 known Lutheran antigens.
 W
WIn Osborn v. Irwin Memorial Blood Bank, 5 Cal.App.4th 234 (1992), the Court of Appeals of California considered certain questions pertaining to whether a blood bank could be held liable for negligence or negligent misrepresentation after a patient contracted HIV/AIDS as a result of a blood transfusion.
 W
WP1PK is a human blood group system based upon the A4GALT gene on chromosome 22. The P antigen was first described by Karl Landsteiner and Philip Levine in 1927. The P1PK blood group system consists of three glycosphingolipid antigens: Pk, P1 and NOR. The GLOB antigen is now the member of the separate GLOB blood group system.
 W
WPacked red blood cells, also known as packed cells, are red blood cells that have been separated for blood transfusion. The packed cells are typically used in anemia that is either causing symptoms or when the hemoglobin is less than usually 70–80 g/L. In adults, one unit brings up hemoglobin levels by about 10 g/L. Repeated transfusions may be required in people receiving cancer chemotherapy or who have hemoglobin disorders. Cross matching is typically required before the blood is given. It is given by injection into a vein.
 W
WPlasmapheresis is the removal, treatment, and return or exchange of blood plasma or components thereof from and to the blood circulation. It is thus an extracorporeal therapy.
 W
WPlatelets, also called thrombocytes, are a component of blood whose function is to react to bleeding from blood vessel injury by clumping, thereby initiating a blood clot. Platelets have no cell nucleus; they are fragments of cytoplasm that are derived from the megakaryocytes of the bone marrow, which then enter the circulation. Circulating unactivated platelets are biconvex discoid (lens-shaped) structures, 2–3 µm in greatest diameter. Activated platelets have cell membrane projections covering their surface. Platelets are found only in mammals, whereas in other vertebrates, thrombocytes circulate as intact mononuclear cells.
 W
WPlatelet transfusion, also known as platelet concentrate, is used to prevent or treat bleeding in people with either a low platelet count or poor platelet function. Often this occurs in people receiving cancer chemotherapy. Preventive transfusion is often done in those with platelet levels of less than 10 x 109/L. In those who are bleeding transfusion is usually carried out at less than 50 x 109/L. Blood group matching (ABO, RhD) is typically recommended before platelets are given. Unmatched platelets, however, are often used due to the unavailability of matched platelets. They are given by injection into a vein.
 W
WPlatelet-rich plasma (PRP), also known as autologous conditioned plasma, is a concentrate of platelet-rich plasma protein derived from whole blood, centrifuged to remove red blood cells. Though promoted to treat an array of medical problems, evidence for benefit is mixed as of 2020, with some evidence for use in certain conditions and against use in other conditions. The cost per injection is generally $US 500 to 2,000 as of 2019.
 W
WPlateletpheresis is the process of collecting thrombocytes, more commonly called platelets, a component of blood involved in blood clotting. The term specifically refers to the method of collecting the platelets, which is performed by a device used in blood donation that separates the platelets and returns other portions of the blood to the donor. Platelet transfusion can be a life-saving procedure in preventing or treating serious complications from bleeding and hemorrhage in patients who have disorders manifesting as thrombocytopenia or platelet dysfunction. This process may also be used therapeutically to treat disorders resulting in extraordinarily high platelet counts such as essential thrombocytosis.
 W
WPostpartum bleeding or postpartum hemorrhage (PPH) is often defined as the loss of more than 500 ml or 1,000 ml of blood within the first 24 hours following childbirth. Some have added the requirement that there also be signs or symptoms of low blood volume for the condition to exist. Signs and symptoms may initially include: an increased heart rate, feeling faint upon standing, and an increased breathing rate. As more blood is lost, the woman may feel cold, blood pressure may drop, and she may become restless or unconscious. The condition can occur up to six weeks following delivery.
 W
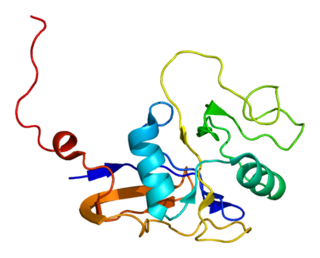
WRh-associated glycoprotein (RHAG) is an ammonia transporter protein that in humans is encoded by the RHAG gene. RHAG has also recently been designated CD241. Mutations in the RHAG gene can cause stomatocytosis.
 W
WSelective immunoglobulin A (IgA) deficiency (SIgAD) is a genetic immunodeficiency, a type of hypogammaglobulinemia. People with this deficiency lack immunoglobulin A (IgA), a type of antibody that protects against infections of the mucous membranes lining the mouth, airways, and digestive tract. It is defined as an undetectable serum IgA level in the presence of normal serum levels of IgG and IgM, in persons older than 4 years. It is the most common of the primary antibody deficiencies. Most such persons remain healthy throughout their lives and are never diagnosed.
 W
WSemaphorin 7A, GPI membrane anchor (SEMA7A) also known as CD108, is a human gene.
 W
WTranexamic acid (TXA) is a medication used to treat or prevent excessive blood loss from major trauma, postpartum bleeding, surgery, tooth removal, nosebleeds, and heavy menstruation. It is also used for hereditary angioedema. It is taken either by mouth or injection into a vein.
 W
WTransfusion-related acute lung injury (TRALI) is a serious blood transfusion complication characterized by the acute onset of non-cardiogenic pulmonary edema presenting with hypoxia following transfusion of blood products.
 W
WTwin-to-twin transfusion syndrome (TTTS), also known as feto-fetal transfusion syndrome (FFTS), twin oligohydramnios-polyhydramnios sequence (TOPS) and stuck twin syndrome is a complication of disproportionate blood supply, resulting in high morbidity and mortality. It can affect monochorionic multiples, that is, multiple pregnancies where two or more fetuses share a chorion and hence a single placenta. Severe TTTS has a 60–100% mortality rate.
 W
WArnault Tzanck (1886–1954) was a French physician and a pioneer of blood transfusion. During the First World War, he was a doctor in the military ambulance where he realized the vital role of the blood transfusions.
 W
WWhole blood (WB) is human blood from a standard blood donation. It is used in the treatment of massive bleeding, in exchange transfusion, and when people donate blood to themselves. One unit of whole blood brings up hemoglobin levels by about 10 g/L. Cross matching is typically done before the blood is given. It is given by injection into a vein.