 W
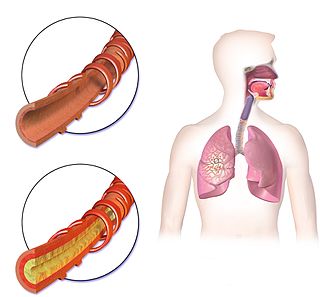
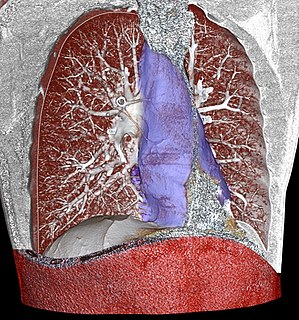
WRespiratory diseases, or lung diseases, are pathological conditions affecting the organs and tissues that make gas exchange difficult in air-breathing animals. They include conditions of the respiratory tract including the trachea, bronchi, bronchioles, alveoli, pleurae, pleural cavity, and the nerves and muscles of respiration. Respiratory diseases range from mild and self-limiting, such as the common cold, influenza, and pharyngitis to life-threatening diseases such as bacterial pneumonia, pulmonary embolism, tuberculosis, acute asthma, lung cancer, and severe acute respiratory syndromes, such as COVID-19. Respiratory diseases can be classified in many different ways, including by the organ or tissue involved, by the type and pattern of associated signs and symptoms, or by the cause of the disease.
 W
WAllergies in children are those causes, pathophsiology, treatments, management, practices and control of allergies that develop in children. Up to 40 percent of children suffer from allergic rhinitis. And children are more likely to develop allergies if one or both parents have allergies. Allergies differ between adults and children. Part of the reason for this that the respiratory system in children is smaller. The bronchi and bronchioles are narrower so even a slight decrease in diameter of these airways can have serious consequences. Many children outgrow their allergies.
 W
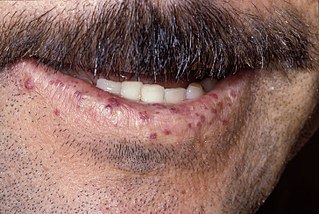
WAllergies, also known as allergic diseases, are a number of conditions caused by hypersensitivity of the immune system to typically harmless substances in the environment. These diseases include hay fever, food allergies, atopic dermatitis, allergic asthma, and anaphylaxis. Symptoms may include red eyes, an itchy rash, sneezing, a runny nose, shortness of breath, or swelling. Food intolerances and food poisoning are separate conditions.
 W
WAnaphylaxis is a serious allergic reaction that is rapid in onset and may cause death. It typically causes more than one of the following: an itchy rash, throat or tongue swelling, shortness of breath, vomiting, lightheadedness, low blood pressure, and temporary blindness. These symptoms typically come on over minutes to hours.
 W
WAtelectasis is the collapse or closure of a lung resulting in reduced or absent gas exchange. It is usually unilateral, affecting part or all of one lung. It is a condition where the alveoli are deflated down to little or no volume, as distinct from pulmonary consolidation, in which they are filled with liquid. It is often called a collapsed lung, although that term may also refer to pneumothorax.
 W
WPeter John Barnes, FRCP, FCCP, FMedSci, FRS is a British respiratory scientist and clinician, a specialist in the mechanisms and treatment of asthma and chronic obstructive pulmonary disease (COPD). He is currently Margeret Turner-Warwick Professor of Thoracic Medicine at the National Heart & Lung Institute, previous head of respiratory medicine at Imperial College and honorary consultant physician at the Royal Brompton Hospital London.. Most highly cited medical researcher in the world.
 W
WCentral hypoventilation syndrome (CHS) is a sleep-related breathing disorder that causes ineffective breathing, apnea, or respiratory arrest during sleep. CHS can either be congenital (CCHS) or acquired (ACHS) later in life. The condition can be fatal if untreated. CCHS was once known as Ondine's curse.
 W
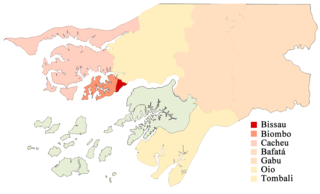
WThe COVID-19 pandemic in Guinea-Bissau is part of the worldwide pandemic of coronavirus disease 2019 caused by severe acute respiratory syndrome coronavirus 2. The virus was confirmed to have reached Guinea-Bissau in March 2020.
 W
WDiffuse panbronchiolitis (DPB) is an inflammatory lung disease of unknown cause. It is a severe, progressive form of bronchiolitis, an inflammatory condition of the bronchioles. The term diffuse signifies that lesions appear throughout both lungs, while panbronchiolitis refers to inflammation found in all layers of the respiratory bronchioles. DPB causes severe inflammation and nodule-like lesions of terminal bronchioles, chronic sinusitis, and intense coughing with large amounts of sputum production.
 W
WDrowning is a type of suffocation due to submersion or immersion of the mouth and nose in a liquid, usually water. The fatal drowning of an individual typically occurs in solitude, or in situations where others are either unaware of the victim's situation, or unable to offer assistance. In the event of a successful resuscitation, victims may experience breathing problems, vomiting, confusion, or unconsciousness. Occasionally, victims may not begin experiencing these symptoms for several hours after they have been rescued. An incident of drowning can also cause further complications for victims due to low body temperature, aspiration of vomit, or acute respiratory distress syndrome.
 W
WObliterative bronchiolitis (OB), also known as constrictive bronchiolitis and popcorn lung, is a disease that results in obstruction of the smallest airways of the lungs (bronchioles) due to inflammation. Symptoms include a dry cough, shortness of breath, wheezing and feeling tired. These symptoms generally get worse over weeks to months. It is not related to cryptogenic organizing pneumonia, previously known as bronchiolitis obliterans organizing pneumonia.
 W
WHamman's syndrome, also known as Macklin's syndrome, is a syndrome of spontaneous subcutaneous emphysema and pneumomediastinum, sometimes associated with pain and, less commonly, dyspnea, dysphonia, and a low-grade fever.
 W
WHemoptysis is the coughing up of blood or blood-stained mucus from the bronchi, larynx, trachea, or lungs. In other words, it is the airway bleeding. This can occur with lung cancer, infections such as tuberculosis, bronchitis, or pneumonia, and certain cardiovascular conditions. Hemoptysis is considered massive at 300 mL. In such cases, there are always severe injuries. The primary danger comes from choking, rather than blood loss.
 W
WHereditary hemorrhagic telangiectasia (HHT), also known as Osler–Weber–Rendu disease and Osler–Weber–Rendu syndrome, is a rare autosomal dominant genetic disorder that leads to abnormal blood vessel formation in the skin, mucous membranes, and often in organs such as the lungs, liver, and brain.
 W
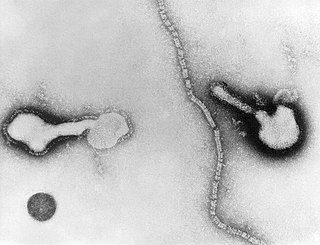
WHuman parainfluenza viruses (HPIVs) are the viruses that cause human parainfluenza. HPIVs are a paraphyletic group of four distinct single-stranded RNA viruses belonging to the Paramyxoviridae family. These viruses are closely associated with both human and veterinary disease. Virions are approximately 150–250 nm in size and contain negative sense RNA with a genome encompassing about 15,000 nucleotides.
 W
WHypercapnia (from the Greek hyper = "above" or "too much" and kapnos = "smoke"), also known as hypercarbia and CO2 retention, is a condition of abnormally elevated carbon dioxide (CO2) levels in the blood. Carbon dioxide is a gaseous product of the body's metabolism and is normally expelled through the lungs. Carbon dioxide may accumulate in any condition that causes hypoventilation, a reduction of alveolar ventilation (the clearance of air from the small sacs of the lung where gas exchange takes place). Inability of the lungs to clear carbon dioxide leads to respiratory acidosis. Eventually the body compensates for the raised acidity by retaining alkali in the kidneys, a process known as "metabolic compensation".
 W
WHypoxia is a condition in which the tissues of the body are deprived of the necessary levels of oxygen. This is not to be confused with hypoxemia, which refers to low levels of oxygen in the blood, although the two conditions often occur simultaneously, since a decrease in blood oxygen typically corresponds to a decrease in oxygen in the surrounding tissue. However, hypoxia may be present without hypoxemia, and vice versa, as in the case of infarction.
 W
WInfantile respiratory distress syndrome (IRDS), also called respiratory distress syndrome of newborn, or increasingly surfactant deficiency disorder (SDD), and previously called hyaline membrane disease (HMD), is a syndrome in premature infants caused by developmental insufficiency of pulmonary surfactant production and structural immaturity in the lungs. It can also be a consequence of neonatal infection and can result from a genetic problem with the production of surfactant-associated proteins. IRDS affects about 1% of newborns and is the leading cause of death in preterm infants. The incidence decreases with advancing gestational age, from about 50% in babies born at 26–28 weeks to about 25% at 30–31 weeks. The syndrome is more frequent in males, Caucasians, infants of diabetic mothers and the second-born of premature twins.
 W
WIntrauterine hypoxia occurs when the fetus is deprived of an adequate supply of oxygen. It may be due to a variety of reasons such as prolapse or occlusion of the umbilical cord, placental infarction and maternal smoking. Intrauterine growth restriction may cause or be the result of hypoxia. Intrauterine hypoxia can cause cellular damage that occurs within the central nervous system. This results in an increased mortality rate, including an increased risk of sudden infant death syndrome (SIDS). Oxygen deprivation in the fetus and neonate have been implicated as either a primary or as a contributing risk factor in numerous neurological and neuropsychiatric disorders such as epilepsy, attention deficit hyperactivity disorder, eating disorders and cerebral palsy.
 W
WKennel cough, also known as canine infectious respiratory disease, formerly canine infectious tracheobronchitis, is an upper respiratory infection affecting dogs. There are multiple causative agents, the most common being the bacterium Bordetella bronchiseptica, followed by canine parainfluenza virus, and to a lesser extent canine coronavirus. It is highly contagious; however adult dogs may display immunity to reinfection even under constant exposure. Kennel cough is so named because the infection can spread quickly among dogs in the close quarters of a kennel or animal shelter.
 W
WLaryngotracheal stenosis refers to abnormal narrowing of the central air passageways. This can occur at the level of the larynx, trachea, carina or main bronchi. In a small number of patients narrowing may be present in more than one anatomical location.
 W
WLipid-laden alveolar macrophages, also known as pulmonary foam cells, are cells found in bronchoalveolar lavage (BAL) specimens that consist of macrophages containing deposits of lipids (fats). The lipid content of the macrophages can be demonstrated using a lipid targeting stain like Oil Red O or Nile red. Increased levels of lipid-laden alveolar macrophages are associated with various respiratory conditions, including chronic smoking, gastroesophageal reflux, lipoid pneumonia, fat embolism, pulmonary alveolar proteinosis and pulmonary aspiration. Lipid-laden alveolar macrophages have been reported in cases of vaping-associated pulmonary injury.
 W
WMediastinal fibrosis most common cause is idiopathic mediastinal fibrosis; less commonly histoplasmosis tuberculosis or unknown. It is characterized by invasive, calcified fibrosis centered on lymph nodes that block major vessels and airways. In Europe, this disease is exceptionally rare. More cases are seen in USA where the disease may often be associated with histoplasmosis.
 W
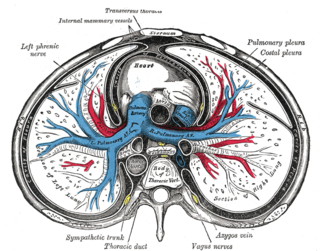
WMediastinitis is inflammation of the tissues in the mid-chest, or mediastinum. It can be either acute or chronic. It is thought to be due to four different etiologies:direct contamination hematogenous or lymphatic spread extension of infection from the neck or retroperitoneum extension from the lung or pleura
 W
WObesity hypoventilation syndrome (OHS) is a condition in which severely overweight people fail to breathe rapidly or deeply enough, resulting in low oxygen levels and high blood carbon dioxide (CO2) levels. The syndrome is often associated with obstructive sleep apnea (OSA), which causes periods of absent or reduced breathing in sleep, resulting in many partial awakenings during the night and sleepiness during the day. The disease puts strain on the heart, which may lead to heart failure and leg swelling.
 W
WOxygen toxicity is a condition resulting from the harmful effects of breathing molecular oxygen at increased partial pressures. Severe cases can result in cell damage and death, with effects most often seen in the central nervous system, lungs, and eyes. Historically, the central nervous system condition was called the Paul Bert effect, and the pulmonary condition the Lorrain Smith effect, after the researchers who pioneered the discoveries and descriptions in the late 19th century. Oxygen toxicity is a concern for underwater divers, those on high concentrations of supplemental oxygen, and those undergoing hyperbaric oxygen therapy.
 W
WThe pathophysiology of acute respiratory distress syndrome involves fluid accumulation in the lungs not explained by heart failure. It is typically provoked by an acute injury to the lungs that results in flooding of the lungs' microscopic air sacs responsible for the exchange of gases such as oxygen and carbon dioxide with capillaries in the lungs. Additional common findings in ARDS include partial collapse of the lungs (atelectasis) and low levels of oxygen in the blood (hypoxemia). The clinical syndrome is associated with pathological findings including pneumonia, eosinophilic pneumonia, cryptogenic organizing pneumonia, acute fibrinous organizing pneumonia, and diffuse alveolar damage (DAD). Of these, the pathology most commonly associated with ARDS is DAD, which is characterized by a diffuse inflammation of lung tissue. The triggering insult to the tissue usually results in an initial release of chemical signals and other inflammatory mediators secreted by local epithelial and endothelial cells.
 W
WPea soup fog is a very thick and often yellowish, greenish or blackish fog caused by air pollution that contains soot particulates and the poisonous gas sulphur dioxide. This very thick smog occurs in cities and is derived from the smoke given off by the burning of soft coal for home heating and in industrial processes. Smog of this intensity is often lethal to vulnerable people such as the elderly, the very young and those with respiratory problems. The result of these phenomena was commonly known as a London particular or London fog; in a reversal of the idiom, "London particular" became the name for a thick pea and ham soup.
 W
WPleural thickening is an increase in the bulkiness of one or both of the pulmonary pleurae.
 W
WPleuropneumonia is inflammation of the lungs and pleura, pleurisy being the inflammation of the pleura alone.
 W
WPneumomediastinum is pneumatosis in the mediastinum. First described in 1819 by René Laennec, the condition can result from physical trauma or other situations that lead to air escaping from the lungs, airways, or bowel into the chest cavity.
 W
WPolymer fume fever or fluoropolymer fever, also informally called Teflon flu, is an inhalation fever caused by the fumes released when polytetrafluoroethylene reaches temperatures of 300 °C (572 °F) to 450 °C (842 °F). When PTFE is heated above 450 °C the pyrolysis products are different and inhalation may cause acute lung injury. Symptoms are flu-like with chest tightness and mild cough. Onset occurs about 4 to 8 hours after exposure to the pyrolysis products of PTFE. A high white blood cell count may be seen and chest x-ray findings are usually minimal.
 W
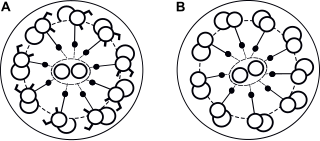
WPrimary ciliary dyskinesia (PCD), is a rare, ciliopathic, autosomal recessive genetic disorder that causes defects in the action of cilia lining the respiratory tract, fallopian tube, and flagellum of sperm cells. The phrase "immotile ciliary syndrome" is no longer favored as the cilia do have movement, but are merely inefficient or unsynchronized.
 W
WPsittacosis—also known as parrot fever, and ornithosis—is a zoonotic infectious disease in humans caused by a bacterium called Chlamydia psittaci and contracted from infected parrots, such as macaws, cockatiels, and budgerigars, and from pigeons, sparrows, ducks, hens, gulls and many other species of birds. The incidence of infection in canaries and finches is believed to be lower than in psittacine birds.
 W
WRespiratory failure results from inadequate gas exchange by the respiratory system, meaning that the arterial oxygen, carbon dioxide or both cannot be kept at normal levels. A drop in the oxygen carried in blood is known as hypoxemia; a rise in arterial carbon dioxide levels is called hypercapnia. Respiratory failure is classified as either Type 1 or Type 2, based on whether there is a high carbon dioxide level, and can be either acute or chronic. The definition of respiratory failure in clinical trials usually includes increased respiratory rate, abnormal blood gases, and evidence of increased work of breathing. Respiratory failure causes an altered mental status due to ischemia in the brain.
 W
WRespiratory risks of indoor swimming pools can include coughing, wheezing, aggravated asthma, and airway hyper-responsiveness. The chemicals used for pool water disinfection can react with organic compounds in the water to create disinfection by-products or DBPs. Exposure to these DBPs are the potential cause for respiratory symptoms in swimmers. Multiple studies have shown the potential correlation between chronic exposure to DBPs and respiratory symptoms among competitive swimmers but more research is needed on the effects of these DBPs on recreational swimmers. The studies on recreational swimmers that have been done show a decreased risk for respiratory symptoms due to a decreased exposure to DBPs. Some studies have been done on the vulnerability of younger children and DBP exposure. Studies done on the vulnerability of younger children demonstrate that immature lungs are more likely to absorb more of these DBPs.
 W
WA respiratory tract infection (RTI) is any number of infectious diseases involving the respiratory tract. An infection of this type is normally further classified as an upper respiratory tract infection or a lower respiratory tract infection. Lower respiratory infections, such as pneumonia, tend to be far more serious conditions than upper respiratory infections, such as the common cold.
 W
WSource control is a strategy for reducing disease transmission by blocking respiratory secretions produced through speaking, coughing, or sneezing. Surgical masks are commonly used for this purpose, with cloth face masks recommended for use by the public only in epidemic situations when there are shortages of surgical masks. In addition, respiratory etiquette such as covering the mouth and nose with a tissue when coughing can be considered source control.
 W
WSubcutaneous emphysema occurs when gas or air travels under the skin. Subcutaneous refers to the tissue beneath the skin, and emphysema refers to trapped air. Since the air generally comes from the chest cavity, subcutaneous emphysema usually occurs on the chest, neck and face, where it is able to travel from the chest cavity along the fascia. Subcutaneous emphysema has a characteristic crackling-feel to the touch, a sensation that has been described as similar to touching Rice Krispies; This sensation of air under the skin is known as subcutaneous crepitation, a form of Crepitus.
 W
WTracheobronchopathia osteochondroplastica (TO) is a rare benign disease of unknown cause, in which multiple cartilaginous or bony submucosal nodules project into the trachea and proximal bronchi. The nodules usually spare the posterior wall of the airway because they are of cartilaginous origin, while the posterior wall of the airway is membranous. This is as opposed to tracheobronchial amyloidosis, which does not spare the posterior wall.
 W
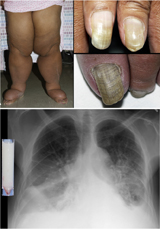
WYellow nail syndrome, also known as "primary lymphedema associated with yellow nails and pleural effusion", is a very rare medical syndrome that includes pleural effusions, lymphedema and yellow dystrophic nails. Approximately 40% will also have bronchiectasis. It is also associated with chronic sinusitis and persistent coughing. It usually affects adults.